Fatty liver can be a silent killer
Non-alcoholic fatty liver disease, which can lead to liver cirrhosis or cancer, on the rise in Singapore
Liver conditions do not just affect alcoholics.
They can be borne from a sedentary lifestyle and when too much fat invades your liver.
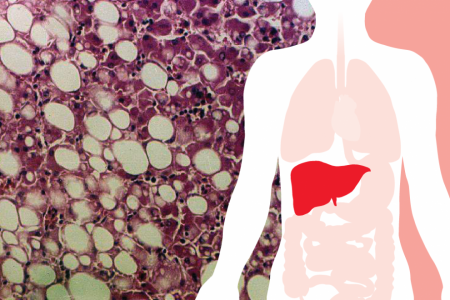
Non-alcoholic fatty liver disease (NAFLD)is an umbrella term for a range of liver conditions from simple fat deposition (non-alcoholic fatty liver) to liver inflammation (non-alcoholic steatohepatitis, also known as Nash) - which is what Punggol East MP and Deputy Speaker Charles Chong was diagnosed with three years ago and had to undergo a liver transplant for.
Globally, one in four adults suffers from fatty liver disease.
In Singapore, there is a "significant increase" in such cases, according to a study published online last December.
The study looked at Singapore General Hospital patients who had surgery to remove their gallbladder, an organ next to the liver, for the periods 2001 to 2004 and 2011 to 2014.
From the pre-operative scans of the earlier group of 127 patients, 40 per cent had NAFLD.
Ten years later, 57 per cent of the 99 patients had it.
More patients in the latter group also had high levels of cholesterol - 46 per cent versus 19 per cent.
Almost half of the patients in both groups had high blood pressure.
A fatty liver is defined as a fat build-up - more than 5 per cent of the liver's total weight - in the liver.
This can affect the normal liver function as the disease progresses, said Dr Kam Juinn Huar, a general surgery consultant at Sengkang Health.
"Repeated liver inflammation in Nash can progress to scarring and hardening of liver (cirrhosis) and eventually liver function may be compromised or fail.
"Some may even develop liver cancer," he told The New Paper.
Risk factors for fatty liver include diabetes mellitus, obesity and hypertension.
EARLY
Early diagnosis and intervention is needed to prevent fatty liver disease from becoming something more serious, like liver cirrhosis or liver cancer.
“Using imaging such as ultrasound, CT and MRI, doctors will be able to see the state of the fatty liver and its complication, if any.”Dr Kam Juinn Huar
Blood tests, while not conclusive, can give a preliminary indication on overall liver function, said Dr Kam.
"Using imaging such as ultrasound, CT and MRI, doctors will be able to see the state of the fatty liver and its complication, if any. Some may require liver biopsy," he added.
But its silent nature - 80 per cent of people with fatty liver are unaware of their condition - means it is often not discovered until it is too late.
In its early stages, fatty liver usually either does not cause any symptoms, or shows up through non-specific symptoms like tiredness, upper abdominal discomfort or nausea.
Only as it progresses to liver cirrhosis do signs grow obvious, such as yellow skin discolouration due to jaundice.
Dr Kam said: "We see many patients regularly who are referred to us only after complications have developed, such as liver cirrhosis or liver cancer.
"At that stage, surgery is more often than not the only effective treatment option."
There is currently no universally accepted medication to treat fatty liver.
The good news is, the progression of NAFLD can be slowed and is reversible when detected in its early stages.
"Losing weight or maintaining a healthy weight, a healthy diet and lifestyle together with regular exercise will help prevent fatty liver," said Dr Kam.
He added that it is also important to treat and control underlying conditions such as diabetes, high cholesterol and hypertension, and maintaining a healthy body weight with appropriate physical activity.
"NAFLD is a condition that is more prevalent than most people are aware of.
"The only way to avoid it is to maintain a healthy lifestyle and regular screening for high-risk individuals," he said.
Get The New Paper on your phone with the free TNP app. Download from the Apple App Store or Google Play Store now